Revita Life Sciences
Osteoarthritis Knee
Osteoarthritis, also known as wear-and-tear or degenerative arthritis, is the most common form of the disease, affecting millions of people each year. This condition is most common in older patients whose cartilage has worn down over time, and in athletes who have worn down their cartilage from overuse and repetitive motions.
Patients with osteoarthritis may experience pain, swelling and stiffness within the joint, which tend to worsen as the condition progresses.
Treatment for osteoarthritis initially focuses on relieving pain and other symptoms, and may include rest, physical therapy, bracing and anti-inflammatory medication. More severe cases of osteoarthritis may require surgery to reposition the bones or replace the joint.
Studies of the use of biologics for cartilage degeneration have shown more consistently favourable results.
INVESTIGATIONS
Cartilage oligomeric matrix protein (СОМР)
Cartilage and bone metabolism markers in patient plasma for OA also known as thrombospondin 5 (TSP 5), is a non-collagen glycoprotein belonging to the extracellular protein family of thrombospondins.
COMP molecules play an important role in maintaining the properties and integrity of the collagen network. It is considered an early marker for the remodeling of articular cartilage.
In OA -COMP, ng/ml 1108 ± 439 In Healthy- 490.0 ± 77.6
Synovial fluid (SF) analysis
- Cytokine analysis:
High level of IL-6, and TNF-α in the synovial fluid.
Baseline in OA -IL6 – 163.5±157.6 (pg/ml) up to 1686.4
Baseline in OA TNF-α 7.2±4.8 (pg/ml) up to 14.8
Inflammatory markers decline in synovial fluid
Baseline -IL6 – 163.5±157.6 (pg/ml) upto1686.4 to After treatment –100-120.
Baseline in OA TNF-α in the synovial fluid. 7.2±4.8 upto 14.8 After treatment 0.6 to 3.0
- Msc and CFU analysis the accumulation of MSCs in SF increases with the severity of osteoarthritis, joint damage, and the disease duration . With OA aggression- a surge of mesenchymal stem cells colony-forming units as apart of tissue response to injury in synovial fluid
Although the source of this MSC increase has not yet been determined, the most likely origin of the increased presence of MSC in SF of OA patients might be the SM, the breakdown zone of superficial AC, and the SB.
Baseline 7.98 ± 8.21 MSC/𝜇L to 1 week -4.04 ± 5.36 MSC/𝜇L (𝑝 = 0.019)
Cfu baseline 601.75 ± 312.30 Cfu 1 week 139.19 ± 123.61 (𝑝 = 0.012)
The presence of mesenchymal stem cells in synovial fluid and colony-forming cells decreases one week after treatment .
Ultrasound
Evidence from recent studies indicates that synovitis plays a critical role in the symptomatic and
Synovial hypertrophy score using a semi-quantitative system grade ranging from 0 (absent) to 3 (severe). While the extent of synovial vascularity graded from 1 (minimal perfusion) to 4 (marked perfusion) presence of Effusion and volume.
In OA Medial jsw around 2 mm Lateral jsw around 4 mm
X ray-
The prevalence of bone attrition 30 to 38%, bone marrow lesions 50-59%,subchondral cysts 23% -31%
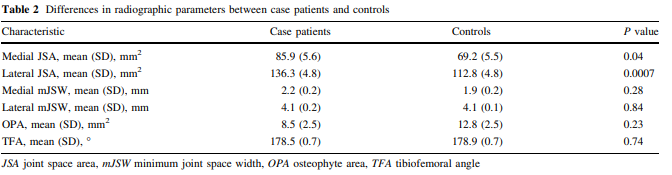
MRI –
MRI detected abnormalities in 72% of patients with cartilage problems who had pain, but so did 68% of those without knee pain.
For quantitative assessment esp important in post procedure followups these programmes give netter understanding of cartilage physiology and morphology
- (WORMS) Whole-Organ Magnetic Resonance Imaging Score
- (BLOKS) Boston-Leeds Osteoarthritis Knee Scores
- 2D and 3D FSE
- dGEMRIC
- T1rho
Indication for Application of Biologics
Symptomatic Knee OA
Grade II to IV
Axial deformity < 5 ° Mechanical deformity (diaphyseal varus of 4 degree, valgus of 16 degree)
Body mass index between 20 and 33
IMC: 20 –30β-HCG = 0
PRP
7x (10 billion ) 8 ml ingle injection leucocyte poor PRP:
- BMAC OR ADSC or MSCs
Total CFU-F, 3-4 x 104
Total CFU-O, 10x 104
Total CFU-C, 10x 104
Nucleated cells 1x 109 to 1x 1011
Addressing bone marrow lesions by Intraosseous Infiltration
In patients with severe OA, the subchondral bone undergoes changes which include microcracks and structural changes, including a progressive replacement of the subchondral marrow with fibro-neurovascular -mesenchymal tissue.it is not just bone odema but areas of medullary fat necrosis, fibrosis, trabecular microfractures, and poor mineralization sclerosis, of subchondral bone.
- Minimal true oedema
- Extensive fibrosis, areas of osteonecrosis
- Does NOT resolve with time
- correlated with worsening knee pain and cartilage loss
- Nine times more likely to require TKA within 3 years than patients without BMLs.
BMLs can also be considered a predictor of the onset of cartilage degradation and the emergence of pain
MRI – high signal on fluid-sensitive sequences of MRI .Other typically observed features include microcracks, micro-oedema, microbleeding, and bone cyst formation within the subchondral region.
SCORING byWhole-Organ Magnetic Resonance Imaging Score (WORMS)
0 points – no BML
1 point – minimally expressed BML (Ø < 5 mm)
2 points – moderate BML (5 mm≤ Ø ≤ 20 mm)
3 points – severe BML (Ø> 20 mm) [
BMLs larger than 1 cm2 are seen in OA patients who report severe pain
TREATMENT
Besides treatment with prostacyclin, bisphosphonates, Protected weight bearing and physiotherapyIntraosseous PRP or biologics to Address the lesion is the best treatment modality these days.
Intra-osseous infiltrations of biologics do not expect to regenerate bone but also to stimulate the subchondral bone (SB) in order to improve the joint biological environment.
Intra-osseous infiltration at same common key points in subchondral bone or at specific BML
Intra-osseous infiltration of biologics targets AC, SF, SM & SB.
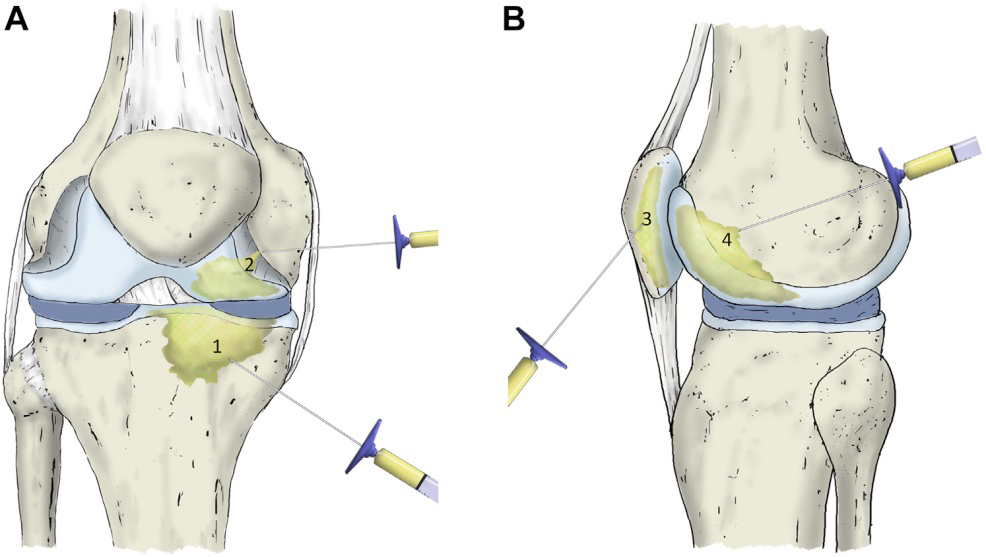
14 Gneedle manually introduced into the bone and inserted 1-2 cm into the medial tibial plateau and medial femoral condyle at an angle of 30–40° to the lower limb anatomical axis.
Once the trocars are placed in the proper position, the needle core was extracted upto 5 ml of biologics infiltrated into the subchondral bone of each structure.
***Hard to infiltrate more than 2 ml into the subchondral bone because of the over-large resistance Sometimes may be because the needle tip too close to the subchondral bone.
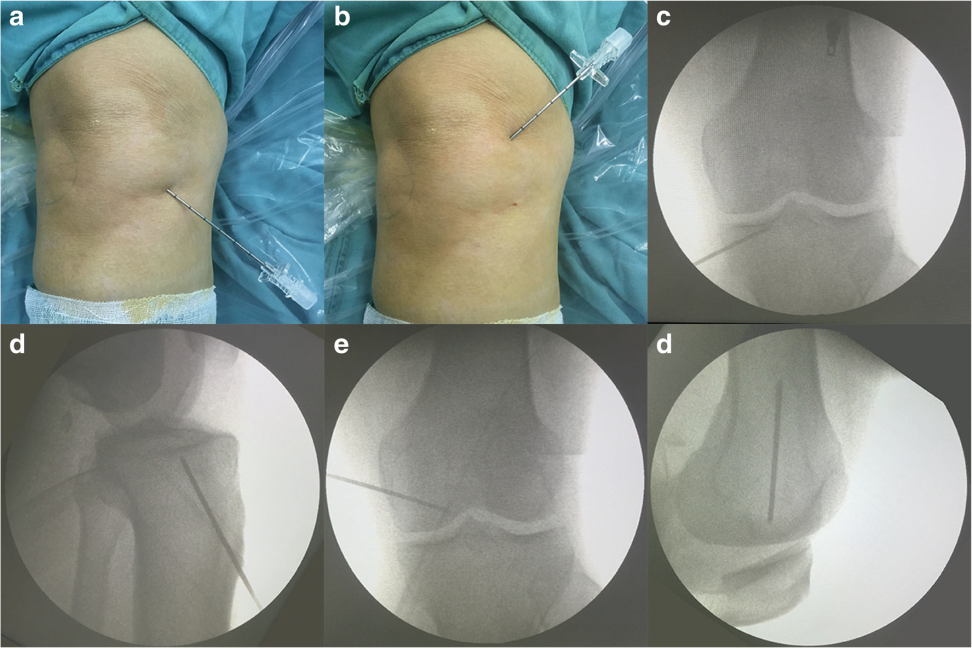
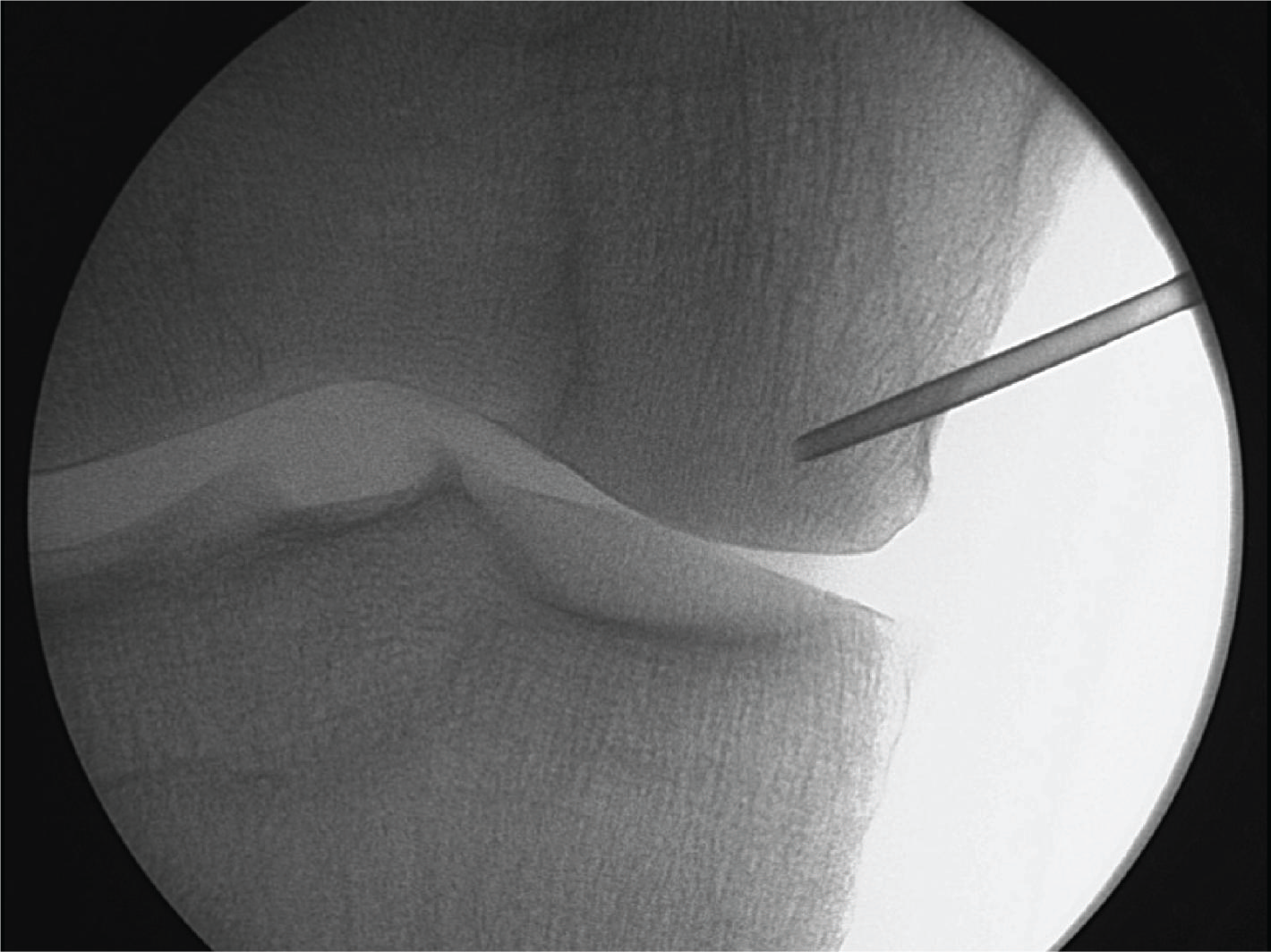
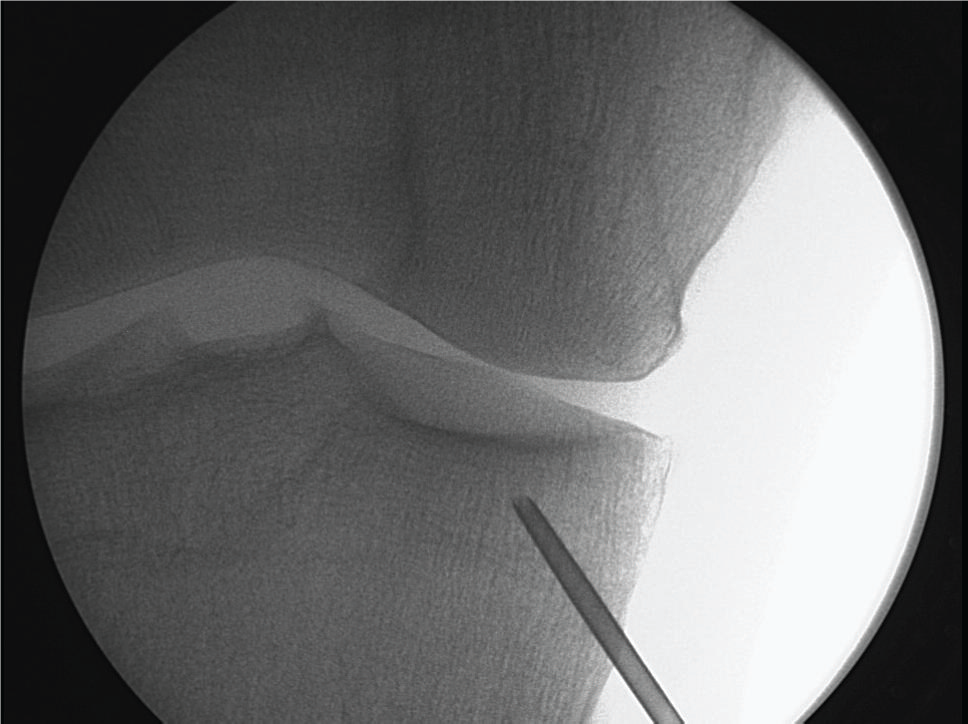
Intraosseous ifilteration at Specific BML sites :
Pre-identified BML area,
Under fluoroscope control by placing a 14 g needle 1 cm close to the subchondral bone.
Addition of core decompression improves outcome many fold.






